"Les photographes s'occupent de choses qui disparaissent continuellement et quand elles ont disparu, rien sur terre ne peut les faire revenir."
the
j o u r n a l
maternity
newborn
collections
galleries
explore
- Henri Cartier Bresson
j o u r n a l
Henri Cartier Bresson
the
"Les photographes s'occupent de choses qui disparaissent continuellement et quand elles ont disparu, rien sur terre ne peut les faire revenir."
Breast Hypoplasia & Insufficient Glandular Tissue (IGT)
As a woman who has (self diagnosed) breast hypoplasia, I had no idea how it would affect my breastfeeding journey with my children. The lactation nurses who saw me also had no idea. The first lactation consultant that I saw as a first time mom after the 16 hour labor with my firstborn took one look at my chest and said
“I’ve never seen this before. Your baby might have difficulty given the shape of your breasts.”
I felt like a a carnival exhibit with the way that she stared appallingly at my chest. Her words were far from comforting, but her words came from an “expert” in a white lab coat, and I was just an exhausted, terrified, and clueless mom. So, I believed her.
Breast Hypoplasia is a condition caused by breast tissue not proliferating properly during puberty, also known as tuberous breasts. Hypoplastic breasts tend to have a gap of more than 1.5 inches between them. Instead of a round appearance, and may appear to be oval, pointed, or square shaped.
There is currently not a lot of information out there about breast hypoplasia and the deep dive that I’ve done scouring the internet for information only unearthed articles saying that it’s “uncommon,” “an abnormality,” “unsuitable for breastfeeding,” and plugs for cosmetic breast augmentation as the only “cure.”
Most experts have aligned Breast Hypoplasia with Insufficient Glandular Tissue (IGT), with the assumption that due to hypoplasia, there are insufficient mammary glands to produce the amount of milk necessary to exclusively breastfeed.
The crazy thing is, I had never heard of breast hypoplasia prior to doing research on my own. No doctor, nurse, or lactation consultant had ever looked at my breasts and said “You have breast hypoplasia.” This was the body that I was born with. I had always known that my breasts looked different than what I had seen in the media, but I never thought of it as a shameful abnormality to be “fixed.”
Just look at this stock image easily found on Google illustrating the “perfect” breast shape.
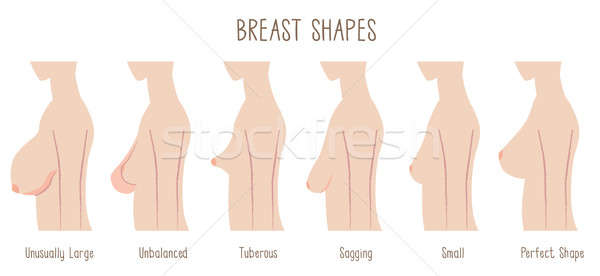
We live in a society that holds female bodies and female body parts to a disgustingly impossible standard.
I’ve already recounted part I of my breastfeeding journey with my daughter and her newborn jaundice, so with my son, I was determined to do everything right. I was determined to learn from my mistakes.
Unfortunately, he too was diagnosed with high levels jaundice and needed monitoring when he was born. I was told, once again, that he needed to be supplemented with formula in addition to breastmilk and again, was told that I might not be able to exclusively breastfeed.
I was pumping around the clock. I would nurse him and Alex would supplement with a tiny syringe of formula, and then I would pump for 15 minutes on each breast, every 2 hours to maintain supply. We did this for almost one month, until my nipples were cracked and bleeding. I would cry from the pain and the exhaustion everytime we nursed.
Ellias’ bilirubin levels were very slowly plateauing but he was still constantly crying, fussing, and unhappy. I was afraid that I wasn’t producing enough for him so when I went to the lactation consultant for my 3rd consultation, she told me that I probably didn’t have enough and that I should lower my expectations for “breastfeeding success.”
I have now breastfed my son for 18 months and counting.
It turns out that what she had interpreted as cries of hunger when we had gone in to see her, were simply cries of fatigue. With the guests we had at home, the doctor visits, and the jaundice, he was screaming because he was tired. Milkwise, he was receiving enough from me alone, even though I was still pumping 3 oz total per feed.
I write all of this so that mamas out there in a similar predicament as me can be encouraged.
You are perfect for your baby. Your body created this child, and your body can do amazing things.
Exclusive breastfeeding is not for everyone, and I support whatever you decide is best for you & your baby. Fed is best, whatever that looks like.
Personally, exclusive breastfeeding was important to me. I am glad that there are now more resources and support than ever before for mothers who would like to exclusively breastfeed. But unfortunately, there is still so much that the medical community does not know about lactation and breastfeeding in general, especially when it comes to breast hypoplasia.
If you have breast hypoplasia and suspect that you may have insufficient glandular tissue, I encourage you to speak with someone about it. Having hypoplastic or tuborous breasts does NOT automatically mean that you have IGT and does NOT mean that you cannot exclusively breastfeed. There is simply not enough information out there yet.
Do the research. Advocate for yourself, and for your baby. Because you and your body are enough, mama! And remember, you are not alone.
Sources
Healthline
https://www.healthline.com/health/tubular-breasts#treatment
Very Well Family
https://www.verywellfamily.com/what-are-hypoplastic-breasts-431773
Medela
https://www.medela.us/breastfeeding/articles/mammary-hypoplasia-what-to-do-if-you-re-diagnosed
KellyMom
https://kellymom.com/bf/got-milk/supply-worries/insufficient-glandular-tissue/
read part i of my story:
breastfeeding & newborn jaundice
"Les photographes s'occupent de choses qui disparaissent continuellement et quand elles ont disparu, rien sur terre ne peut les faire revenir."
the
j o u r n a l
maternity
newborn
collections
galleries
explore
- Henri Cartier Bresson
Investments for your custom Portrait Session begins at $1949.
Fill out my Contact Form to get started!
Upon inquiry, you will receive a Collection Guide of detailed pricing & offers.
Please inquire at least one month prior to your desired Session Date.
Availability for Fall & Holiday Bookings is limited.
I can't wait to hear from you!
LEARN MORE
LEARN MORE
Investment for your custom
Portrait Session begins at $1949.
Fill out my Contact Form to get started!
Upon inquiry, you will receive a Collection Guide of detailed pricing & offers.
Please inquire at least one month prior to your desired Session Date.
Availability for Fall & Holiday Bookings is limited.
I can't wait to hear from you!
about tiffany chi photography
An introductory video
view post
published work
My work has been featured in prominent publications such as La Peche Journal, The Fount Collective, Shoutout Los Angeles, Voyage Los Angeles, and The Motherhood Anthology
view post
Our story
From California, to Paris, to Motherhood.
This is my story.